Theranostics
Both diagnostic molecular imaging and therapy use substances called radiopharmaceuticals. Radiopharmaceuticals consist of a radioactive isotope combined with a specific targeting agent, which seeks out specific clusters of cells in the body (for example certain types of cancer cells).
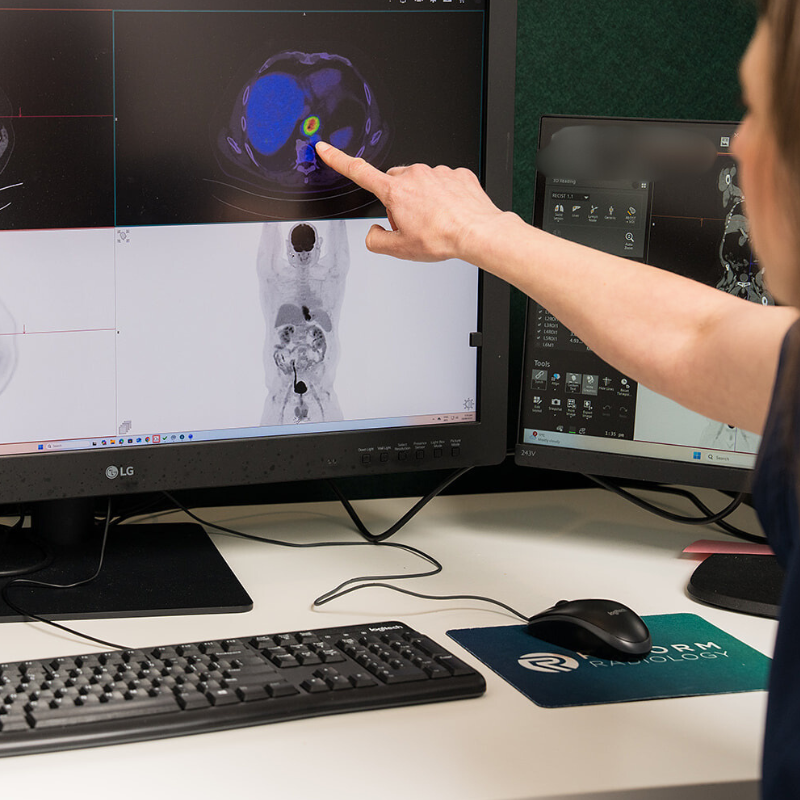
During diagnostic molecular imaging, the radiopharmaceutical contains a relatively low radiation dose radioisotope, combined with a targeting agent which is specially designed to find and highlight abnormal tissue, for example in PET-CT scanning. The images produced are used to localise and stage the extent of disease and allow personalised treatment planning.
In a therapeutic approach, the targeting agent seeks out the same abnormal tissue demonstrated on imaging; however, the radioactive isotope is exchanged for one that delivers therapeutic radiation. In this way, the radiopharmaceutical delivers a treatment dose of radiation to damage the diseased cells, while largely sparing adjacent healthy tissue.
Using a theranostics approach, pairs of radiopharmaceuticals can be used in a complementary way to both diagnose and treat disease in an individualised manner.
Types of nuclear medicine therapies
We offer:
Lutetium-177 therapy
Iodine-131 therapy to patients with thyroid disease.
Other therapies may be available on discussion with your referring doctor or our nuclear medicine specialists.
Theranostics combines diagnosis and therapy of diseases, especially cancer, in a personalised approach to delivering treatment.
Theranostics combines diagnosis and therapy of diseases, especially cancer, in a personalised approach to delivering treatment.
Potential benefits and side effects of nuclear medicine therapy
Goals of nuclear medicine therapy for cancer include reducing the burden of disease, halting the progression of disease, and improving quality of life by reducing associated symptoms. Our nuclear medicine specialists will discuss your individualised treatment plan and goals of therapy with you during your consultation.
Nuclear medicine therapies are generally well tolerated, and your nuclear medicine specialist will offer a personalised discussion around risks and benefits of therapy relevant to you.
Accessing nuclear medicine therapy
To undergo nuclear medicine therapy, you'll need a referral from your oncologist or endocrinologist. You can contact our bookings team on 039625700 or email bookings@reformradiology.co.nz. Our team will help facilitate your appointment.
You will be offered a consultation with one of our nuclear medicine specialists to determine if nuclear medicine therapy is appropriate for you and to set up a treatment plan.
To best determine your treatment plan, additional PET-CT imaging and blood tests may be required.
Inform your healthcare provider and our team of any medications you are taking.
Please let our team know if you are or think you could be pregnant.
What to expect during nuclear medicine therapy
On the day of your therapy the nuclear medicine technologist will infuse the treatment radiopharmaceutical slowly using an automatic intravenous infusion pump. You are likely to be with us for some hours during the treatment. You may also be administered an infusion to protect your kidneys from side effects and receive preventative medication against nausea. When receiving I-131 treatment for thyroid disease, you will instead be asked to swallow the treatment radiopharmaceutical in the form of a tablet.
It is a good idea to bring a book or magazine to help pass the time whilst receiving therapy.
When the therapy session is completed, you will receive information about how to minimise the risk of radiation exposure to your family and community.
Following your therapy session, you will be asked to return to the clinic for a post treatment SPECT-CT scan. This scan is used to evaluate the uptake of the radiopharmaceutical in the tumours and to help guide your future treatments.
You will be offered follow-up blood tests and consultation with our team to monitor your treatment response.
Radiation exposure
Therapeutic radiopharmaceuticals inherently result in radiation doses to patients, with the majority of the dose delivered to tumour tissue. Potential benefits of nuclear medicine therapy should always outweigh the risks of the necessary radiation exposure.